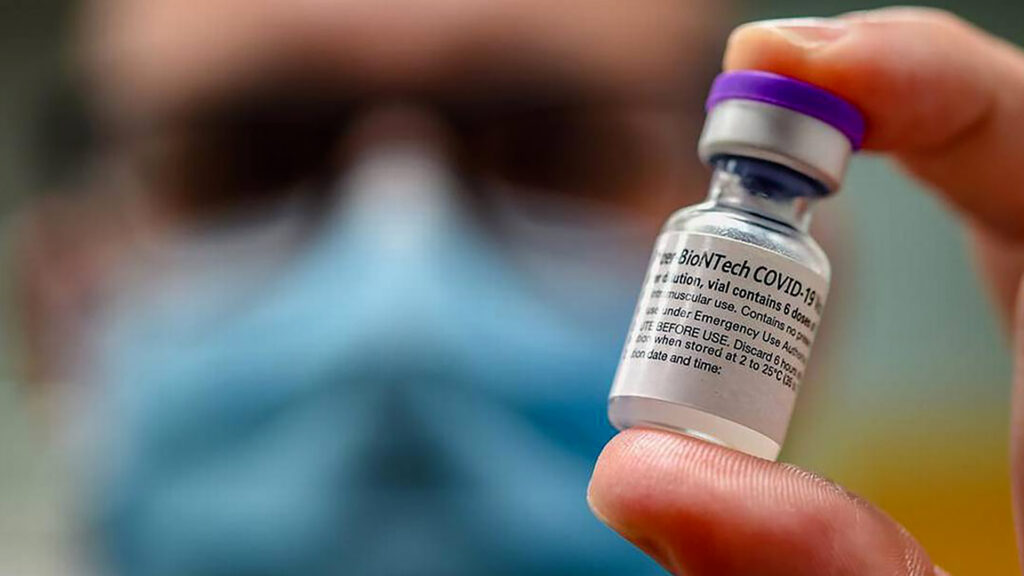
The Food and Drug Administration plans to limit approval of updated COVID-19 vaccines to adults 65 and older and individuals over 6 months old with at least one high-risk health condition. That includes people with asthma, cancer, diabetes, obesity and pregnant women.
Unbiased. Straight Facts.TM
The FDA advises people aged 65 and older to receive two doses of the 2024–2025 COVID-19 vaccine, spaced six months apart. If unvaccinated with Novavax, a third dose is recommended six months after the second.
The change narrows prior universal recommendations and aligns U.S. policy more closely with international approaches.
FDA officials estimate more than 100 million Americans will qualify. However, it remains unclear whether healthy people under 65 can access the vaccine or whether insurers will cover it without a broader recommendation.
Why is the FDA changing its approach to vaccine approvals?
FDA Commissioner Marty Makary and vaccine regulator Vinay Prasad announced the change in the New England Journal of Medicine, arguing that new, randomized clinical trial data should back updated COVID-19 vaccines for healthy people. The policy shift reflects growing immunity levels from prior infections and vaccinations and aims to restore public trust following low booster uptake.
In their article, Makary and Prasad criticized the U.S.’s previous broad vaccine strategy as overly aggressive, suggesting it eroded vaccine confidence, including for illnesses like measles and mumps.
What are the FDA’s requirements for vaccines to move beyond high-risk groups?
Going forward, manufacturers must conduct placebo-controlled trials to seek FDA approval for use in healthy individuals aged 6 months to 64 years. Trials could begin this summer, with preliminary results expected next year. The FDA may still approve shots for high-risk groups while encouraging studies for others.
How have manufacturers and experts responded?
Pfizer and Moderna said they review the FDA’s guidance and remain committed to working with regulators. Both defended the safety and effectiveness of their vaccines, which have been widely administered.
Some experts warned that the policy may limit access for people not classified as high-risk and could impact insurance coverage unless the CDC broadens its recommendations. The CDC’s advisory panel will vote on June 25.
What comes next?
The CDC vote will determine whether the narrower FDA approval becomes national policy. Insurers are required by law to cover CDC-recommended vaccines. The policy change comes amid broader shifts under the Trump administration, which has pushed for stricter testing standards led by Health Secretary Robert F. Kennedy Jr.
contributed to this report.